प्रॉक्सिमल ह्युमरस भागको भंग बुझ्नु
प्रॉक्सिमल ह्युमरस को साइन्डरको चलान र शक्तिमा महत्वपूर्ण भूमिका खेल्दछ, जसले महत्वपूर्ण विशेषताहरू जस्तै ग्रेटर र लेसर ट्यूबेरसिटीहरू र सर्जिकल नेकलाई धारण गर्दछ। यी शरीरीय संरचनाहरू रोटेटर कफ जस्ता मांसपेशी अटैचमेन्ट पॉइंटहरूलाई समर्थन गर्दछ, जसले बाहुको घूमाउन र उठाउनमा सहयोग गर्दछ। प्रॉक्सिमल ह्युमरसको सर्जिकल नेक भंगको एक सामान्य स्थल हो, किनभने यो संकीर्ण संरचनाबाट तनाव वा प्रभावमा भंग हुन सक्दै छ।
प्रॉक्सिमल ह्युमेरस भागमा भंगी विस्थापन र जटिलताको आधारमा वर्गीकृत गरिन्छ: अविस्थापित भंगी, विस्थापित भंगी, र जटिल भंगी। अविस्थापित भंगी सामान्यतया अपनो आनात्मीय सजिलाई बनाए राख्छन् र केही परिस्थितिमा आरोग्यकर उपचार द्वारा उपचित गरिन्छन्, जबकि विस्थापित भंगीमा हड्डीका टुक्राहरू अपनो मूल स्थानबाट फर्किन्छन्, जसले सर्जिकल अनुप्रवेशको आवश्यकता पनि पर्न सक्छ। जटिल भंगीहरू, जो आमतौरमा बृद्ध वयका लागि निम्न हड्डी खनिज घनत्वकारण देखिन्छ, हड्डी संरचनालाई महत्वपूर्ण रूपमा बाधित गर्न सक्छ र उनीहरूलाई मैक्सिलोफेसियल प्लेटहरू जस्ता उन्नत सर्जिकल ठेसन प्रक्रियाहरूले स्थिर बनाउन सकिन्छ।
यी भाग्नाहरू ६५ वर्षभन्दा बढी वयको व्यक्तिहरूमा तीस्रो सबैभन्दा अधिक छन्, जसले वय र लिङ्गमा चमत्कारपूर्ण झुकाव देखाउँछ। महिलाहरू, विशेषगरी ऐस्टियोपोरोसिसको साथीहरू, प्राय: प्रसारण भाग्नाहरूमा अधिक प्रवण हुन्छन्, जसले आम्बाले गिराएको वा क्रीडा घाटीबाट परिणामित हुन सक्छ। हालको मार्फतिक डाटाबाट, यी भाग्नाहरूको घटनाक्रम वृद्ध वयको मध्ये प्रति वर्ष १५% बढी छ, जसले फेमोरल नेक भाग्नाहरूसँग एकजुट सार्वजनिक स्वास्थ्यको बारेमा बडी चिन्ता दिन्छ।
ह्युमरसको महत्व एकअर्कामा बाँधिएका नाखूनहरू
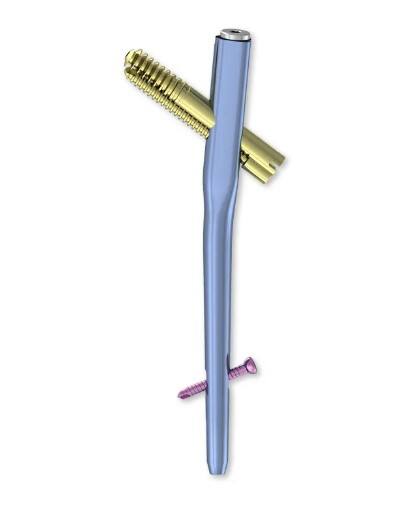
ह्युमरस इन्टरलॉकिङ नेलहरू भाग्ना स्थिरीकरणमा केही फाइदाहरू प्रदान गर्दछन्, विशेषगरी स्थिरतालाई बढाउँदछ, जटिलतालाई कमाउँदछ र अघि गतिशीलतालाई समर्थन गर्दछ। पारंपरिक पद्धतिहरूको बिरुद्ध, यी नेलहरू रगत्तीको अक्षमा भाग्नाहरूलाई स्थिर बनाउँछन्, भारलाई प्रभावी रूपमा वितरण गर्दछन् र समायोजन बनाउँछन्। यसले तेजीमा बाढो समय र कठिनाईहरूबाट पुनर्प्रस्ताव गर्ने घटनाहरूमा कमी लाग्छ।
जब हामी ह्युमरसलाई अन्य फिक्सिङ विधिहरू जस्तै प्लेट र स्क्रूसँग तुलना गर्छौं, तब भिन्नता स्पष्ट हुन्छ। प्लेट र स्क्रूले प्रायः गैर जटिल फ्र्याक्चरहरूमा पर्याप्त स्थिरता प्रदान गर्दछ तर जटिल फ्र्याक्चरहरूमा घाँटी-शाफ्ट कोण कायम गर्न कम हुन सक्छ, जसले मेकानिकल विफलता निम्त्याउन सक्छ। यसको विपरीत, एकअर्कामा बाँधिएका नङहरूले उच्च भार सहन सक्ने क्षमता प्रदान गर्छन्, जुन जटिल फ्र्याक्चरको लागि महत्त्वपूर्ण छ, जसको परिणाम स्वरूप निको हुने क्रममा सुधार हुन्छ।
बायोमेकेनिकल मान्यताहरू फिक्सेशन पद्धति का चयनमा महत्वपूर्ण प्रभाव गर्दछ। इन्टरलॉकिङ नेलहरू भंगुवट ठाउँमा समान भार वितरण सुनिश्चित गर्छन्, जसले समानान्तर राख्न वा मल्युनियन हुन सम्भाव्यता घटाउनमा मद्दत गर्दछ। प्लेटहरू, जबजब प्रभावी छन्, अक्षीय स्थिरतामा एउटै स्तरको समानता प्रदान गर्न सक्दैनन्, बिशेषगरी ऑस्टिओपोरोसिस अस्थिहरूमा वा जटिल भंगुवट विन्यासहरूमा। सही चयन भंगुवटका विशिष्ट विशेषताहरू र पेशिलाई समग्र स्वास्थ्यमा निर्भर गर्छ, जसले ऑर्थोपेडिक उपचार पद्धतिमा व्यक्तिगत पद्धतिको महत्व दर्शाउँछ।
Best Humerus एकअर्कामा बाँधिएका नाखूनहरू प्रॉक्सिमल ह्युमेरस भंगुवटहरूका लागि
प्रॉक्सिमल ह्युमेरस भंगुवटहरूका लागि राम्रो ह्युमेरस इन्टरलॉकिङ नेलहरू चयन गर्दा केही महत्वपूर्ण बिन्दुहरू ध्यानमा राख्न सकिन्छ उत्पादनहरू विशेषताहरू र फाइदाहरूको आधारमा प्रमुख हुन्छन्। यी सामग्रीहरू आमतौरे सुरक्षित र प्रभावशाली हुन सक्ने उन्नत सामग्रीहरूसँग बर्खास्त गर्दछन्, जसले जैविक संगतता र कारोज्ञातिरोधी गुणहरू प्रदान गर्दछ, जस्तै कि टायटेनियम वा स्टेनलेस स्टील। डिझाइनमा उन्नतिहरू मानव अस्थिको प्राकृतिक शारीरिक संरचनामा फिट हुने चिकनाएर आकारहरू समेत छन्, जसले सर्जरीको समय कम गर्दछ र स्थिरतालाई बढाउँछ। अझ यी नेलहरू पेशिक संगतताको लागि डिझाइन गरिएका छन्, जसले विभिन्न पेशिक शारीरिक संरचनाहरू र विशिष्ट भंगिहरूको लागि आकारहरू प्रदान गर्दछ, जसले राम्रो फिटिङ्ग र भरपुर गर्ने परिणामलाई प्रोत्साहन दिन्छ।
कैफियती परिणामहरू आधारित शीर्ष ह्युमेरस अन्तःजालीय केलालहरू उनीहरूको उच्च सफलता दर, रोगी सन्तुष्टि र मिनिमल पछाडी संचालन जटिलताहरूद्वारा भेदित छन्। यी शीर्ष निवडहरू क्रियात्मक परीक्षणहरूमा महत्वपूर्ण फाइदाहरू दर्शाउने गर्छन्, जसले तेस्रो समयमा बढी ठूलो पुनर्स्थापना र जैस्को संक्रमण वा केलाल पलायन जस्ता जटिलताहरूको दरमा कम दर देखाउँछ। जार्नल ऑफ म्युस्कुलोस्केलिटल डिसऑर्डर्समा प्रकाशित एक अध्ययनअनुसार, अग्रणी अन्तःजालीय केलाल मॉडेलहरूको सफलता दर ९०% भन्दा बढी हुन सक्छ, जहाँ कई रोगीहरूले संचालनपछि सुधारित गतिशीलता र दर्दमा कमी पाउने हुन्छ।
विशेषज्ञहरूको सुझाबले क्लिनिकल चिकित्सकहरूलाई अंतःसंधान नेलहरूको चयनमा मार्गदर्शन गर्ने महत्वपूर्ण भूमिका खेल्दछ। प्रसिद्ध अस्थिचिकित्सा शल्यचिकित्सकहरूले रोगीको अस्थिगुणस्तर, भाग्नाको जटिलता र नेलको बायोमेकेनिकल गुणस्तरहरूलाई ध्यानमा राखेर चयन गर्न सल्लाह दिन्छ। प्रमुख अस्थिचिकित्सा विशेषज्ञ, डॉ॰ जॉन स्मिथले रोगीको भाग्नास्थानमा थोरै आंदोलन दिने गरी भाग्नाको ठीक लाग्नमा मद्दत गर्ने ऐसा नेल प्रयोग गर्ने सल्लाह दिन्छ। अन्यथा, उद्योगको मानकहरूले फ्लेक्सिबिलिटी र निश्चितकरणको बीच सही संतुलन प्राप्त गर्ने लॉकिङ विकल्पहरूसह नेल प्रयोग गर्न सल्लाह दिन्छ, जसले रोगीको उत्कृष्ट परिणामको लागि महत्वपूर्ण छ। यी जानकारीहरू विविध निर्णय ग्रहण गर्दै जसले रोगिको लागि सबैभन्दा योग्य अंतःसंधान नेल चयन गर्न चिकित्सकहरूलाई मद्दत गर्दछ।
ह्युमरस लागू गर्ने शल्य तकनीकहरू एकअर्कामा बाँधिएका नाखूनहरू
ह्यूमरस इनटरलॉकिङ नेल्स लगाउन सुकृत शल्य क्रिया पद्धति आवश्यक हुन्छ जसमा केही महत्वपूर्ण कदमहरू अावश्यक छन्। प्रारंभमा, रोगीहरूलाई सामान्य बेचेन्द्रियता तल ठेक्ने हुन्छ, आम्बाले बीच चेयर स्थिति मा। त्यसपछि शल्य प्रयोगले एन्टेरोलैटरल डेल्टॉइड स्प्लिट अप्रोच द्वारा गरिन्छ, मांसपेशी भण्डारहरूको सावधान उपयोग गरेर। त्यसपछि, फ्रैक्चर टुक्राहरूलाई सट्टा लगाउन K-वाइर्स वा बोन हुकहरू जस्ता अस्थायी बन्धन यन्त्रहरू प्रयोग गरिन्छ। त्यसपछि नेल्लाई तयार पन्ना मार्ग मा फेलिन्छ र त्यसपछि फ्रैक्चर स्थिर बनाउन लॉकिङ स्क्रूहरू फेलिन्छ। यो क्रियाकलाप फ्लुओरोस्कोपिक मार्गदर्शनबाट लाभ पाउँछ किनकि यसले अंगठानकको ऑप्टिमल स्थापना पुष्टि गर्दछ र ह्यूमरस शाखासँग ठीक रूपमा समान हुनेछ।
यो शल्यक्रियाको सफलता निर्धारण गर्न रोगीको चयन महत्त्वपूर्ण छ। रोगको उमेर, समग्र स्वास्थ्य र विशिष्ट प्रकारको ह्युमरल फ्र्याक्चर जस्ता मापदण्डले महत्त्वपूर्ण भूमिका खेल्छ। वृद्ध रोगीहरू, वा जटिल फ्र्याक्चर ढाँचाहरू जस्तै बहु-भाग निकटतम humeral फ्र्याक्चरहरूसँग, प्रायः यस विधिबाट सबैभन्दा बढी फाइदा लिन्छन् यसको न्यूनतम आक्रमणकारीता र प्रभावकारी हड्डी स्थिरीकरण गुणहरूको कारण। यी कारकहरूले सामूहिक रूपमा ओर्थोपेडिक सर्जनहरूको निर्णय प्रक्रियालाई प्रभाव पार्छ।
प्रसंगको बादको सorgुरो कार्यक्रम पेशेर बाढी मा अत्यधिक महत्वपूर्ण छ, जसले शारीरिक पुनर्मोड़न र सम्भावित समस्याहरूका लागि पर्यवेक्षण दुई तरिकाले आयोजित गर्दछ। पुनर्मोड़नलाई प्रसंगको एकदिनपछि पनि शुरू गर्न पठाउने पासिभ मोशन अभ्यासबाट शुरू गर्नु पर्दछ, जसले चालन र दर्दको कमजोर हुने साथै सक्रिय-सहायक चालन अभ्यासमा बढ्दछ। पेशेरलाई अतिरिक्त दर्द, फुफ्फुआउने वा चालनको रेंजमा कमी जसले संक्रमण वा डिभाइसको बिफाल्टहरूलाई सूचित गर्न सक्छ, त्यसैगरी लाल झंडा पहिचान गर्न उनीहरूलाई सिखाउनु पर्दछ। ठीक भएको भरपुर भरपुर पुनर्मोड़न र शक्तिमानतालाई जतिएको समयमा पुनर्प्राप्त गर्नका लागि पुनर्मोड़न प्रोटोकोलहरूलाई समायोजित गर्न र ठीक भएको भरपुर भरपुर उपचार गर्न नियमित पछाडी परीक्षणहरू अनिवार्य छन्।
ह्युमरसमा समस्याहरू र चुनौतिहरू एकअर्कामा बाँधिएका नाखूनहरू
ह्युमरस इन्टरलॉकिङ नेलहरूको अपनाईमा केही परेशानिहरू आउन सक्छन्, जसलाई स्वास्थ्य सेवा पेशेवरहरूले ध्यानमा राख्नु पर्दछ। सामान्य परेशानिहरू मेडिकल साइटमा संक्रमण, भएको रूपमा बाटोहरू गलत ढंगै जोडिन्छन् भनेर बदशुद्धि, र बाटोहरू एकसाथ जोडिँदैनन् भनेर अशुद्धि छ। यी परेशानिहरू लामो सुधारको काल देखाउन सक्छन् र अन्य अनुसन्धानहरूको आवश्यकता पनि हुन सक्छ। एक अध्ययन प्रकाशित भएको छ Journal of Bone and Joint Surgery अर्थोपेडिक सर्जरीमा संक्रमण दरहरू पेशिले परिणामहरूमा महत्वपूर्ण रूपमा प्रभाव गर्दछ र सर्जरी प्रोटोकलहरूमा चर्चा गर्न आवश्यक छ।
यी कठिनाइहरूलाई प्रबंधन गर्न बहुमुखी दृष्टिकोणको आवश्यकता पर्दछ। मिलनेमा खराब भएका हालातहरू सच्याउन वा संक्रमणहरूलाई उपचार गर्न सर्जिकल परिचालनहरू आवश्यक पर्न सक्छन्, तसबीक शारीरिक चिकित्साले पुनर्स्थापन र कार्यको पुनः स्थापनमा महत्वपूर्ण भूमिका खेल्दछ। अलि, पछाडी परिचरणको बारेमा शिक्षण पेशिलाई झट्टै झन्डाउने जोखिमहरूलाई कसरी कम गर्ने भएको जान्न गर्न जरुरी छ, जस्तै कि सहायक उपकरणहरूलाई सही रूपमा प्रयोग गर्न र जोखिमहरूका पूर्व लक्षणहरूलाई पहिचान गर्न। चिकित्सा प्रक्रियाहरूमा नवाचारहरू अगाडि जस्तो छ, यी तकनीकहरूले पेशिहरूको चिकित्सालाई विकसित गरी बढाउनको संभावना छ।
अगाडि देखिन्छ, ह्युमरस इनटरलॉकिङ नेलहरू सँग सम्बन्धित जोखिमहरू कम्गर्ने कुछ वातावरणहरू रहेका छन्। बायोअब्सोर्बल माटेरियलहरूको प्रयोग र नेल डिझाइनमा सुधारहरू जसले प्राकृतिक शरीरको आकारलाई बढी रूपमा समायोजन गर्दछन्, यी सबैले भरपुरपछि भर्खर्खो गर्न र जोखिमहरूको दर कमाउन मद्दत गर्न सक्छ। यी माटेरियलहरू र त्यसको अनुप्रयोगमा अनुसंधान फरक पर्ने उपचारहरूमा नयाँ ज्ञानहरू प्रदान गर्न सक्छ, जसले कम जोखिमसहित र बढी सफल परिणामहरूको लागि मार्ग प्रशस्त गर्न सक्छ।
निष्कर्ष र भविष्यको परिप्रेक्ष्य
नतिजा मा, प्रैक्सिमल ह्युमरस भंगको बायोमेकेनिक्सको समज र उपयुक्त फिक्सेशन पद्धतिहरूको चयन गर्न पेशेवरहरूले रोगीहरूको परिणाम अधिक रूपमा उत्कृष्ट बनाउनका लागि महत्वपूर्ण छ। यो लेखले आतंगिक स्थिरता र कम जटिलताहरूको बारेमा चर्चा गर्दछ, जसले भविष्यका उपचारहरूको लागि महत्वपूर्ण आधार प्रदान गर्दछ। नविन झुकावहरू न्यूनतम आक्रमक पद्धतिहरू र तेजीसँग ठीक भएर जान प्रोटोकलहरूको दिशामा छ, जसले प्रैक्सिमल ह्युमरस भंगबाट ग्रस्त रोगीहरूको ठीक भइरहन र परिणामलाई सुधार्नका लागि उद्देश्यमान राहतहरू पेश गर्दछ।
यस क्षेत्रलाई अगाडि बढाउनका लागि अझै पनि अधिक अनुसंधान आवश्यक छ। विभिन्न फिक्सेशन तकनीकहरूको दीर्घकालिन परिणाम र नयाँ इम्प्लांट डिझाइनहरूको विकासमा फोकस गर्ने अनुसंधानहरू महत्वपूर्ण नवाचारहरूमा निवेश गर्न सक्छ। यो निरन्तर अनुसंधानले उपचार पद्धतिहरूलाई अगाडि बढाउने गर्छ, जसले रोगीहरूको सेवामा सुधार र अर्थोपेडिक अभ्यासमा मलुनियन र संक्रमण जस्ता जटिलताहरूको घटत हुन पर्दछ।
सोधिने प्रश्नहरू
प्रॉक्सिमल ह्युमरस भागमा भंग के हो?
प्रॉक्सिमल ह्युमरस भागमा भंग हार्दो में बाहेको ऊपरी हड्डीमा घटियामा नजिकै भइन्छ, जसलाई प्रभावहरू वा गिरानीहरूद्वारा धेरै समय प्रेरित गरिन्छ। यी भंग सामान्यतया अवस्थित भन्दा जटिल मामिलालाई पुग्न सक्छ र निम्न हड्डी घनत्व भएको वृद्ध वयकोमध्ये विशेष रूपमा आम छ।
ह्युमरस इन्टरलॉकिङ नेलहरूलाई यी भंगका लागि सुझाव दिइन्छ किना?
ह्युमरस इन्टरलॉकिङ नेलहरूलाई सुझाव दिइन्छ किनकि तिनीहरू स्थिरता मजबूत बनाउँछन्, भार समान रूपमा वितरण गर्दछन् र प्रारंभिक चलाउने गर्दछन्, जसले प्लेटहरू र स्क्रूहरू जस्ता केही पारंपरिक स्थिरीकरण पद्धतिहरूबाट तुलनात्मक रूपमा तेजीमा बहालीको लागि प्रेरणा दिन्छ।
ह्युमरस इन्टरलॉकिङ नेल छान्नु पर्दा के कारकहरूलाई माथी लिनु पर्दछ?
कारकहरूमा पेशिको हड्डी गुणस्तर, भंगको जटिलता, र नेलको बायोमेकेनिकल गुणस्तरहरू आउन्छ। यो अनिवार्य छ कि तपाईं एक नेल छान्नु होस् जसले पेशिको रचनामा फिट छ र उत्तम रूपमा ठीक भइन्छ।
ह्युमरस इन्टरलॉकिङ नेलहरूसँग सम्बन्धित केही सामान्य जटिलताहरू के हुन सक्छ?
सामान्य कठिनाइहरूमा संक्रमण, गलत संghuchan, र nonunions छन्, जसले बहुदै ठीक भएको समय बढाउन सक्छ र अतिरिक्त उपचारको आवश्यकता पनि उत्पन्न गर्दछ।
ह्युमरस इन्टरलॉकिङ नेलहरूबाट आउने कठिनाइहरूलाई कसरी प्रबंधन गर्न सकिन्छ?
कठिनाइहरूलाई प्रबंधन गर्न सर्जिकल सुधारहरू, पुनर्वासन, र परिचालनपछि देखभाल व्यवस्थाहरूबारे रोगिहरूलाई शिक्षित गर्न आवश्यक छ जसले अर्को कठिनाइहरूलाई जल्दै चर्चा गर्न मद्दत गर्दछ।
सामग्रीको सूची
- प्रॉक्सिमल ह्युमरस भागको भंग बुझ्नु
- ह्युमरसको महत्व एकअर्कामा बाँधिएका नाखूनहरू
- Best Humerus एकअर्कामा बाँधिएका नाखूनहरू प्रॉक्सिमल ह्युमेरस भंगुवटहरूका लागि
- ह्युमरस लागू गर्ने शल्य तकनीकहरू एकअर्कामा बाँधिएका नाखूनहरू
- ह्युमरसमा समस्याहरू र चुनौतिहरू एकअर्कामा बाँधिएका नाखूनहरू
- निष्कर्ष र भविष्यको परिप्रेक्ष्य
-
सोधिने प्रश्नहरू
- प्रॉक्सिमल ह्युमरस भागमा भंग के हो?
- ह्युमरस इन्टरलॉकिङ नेलहरूलाई यी भंगका लागि सुझाव दिइन्छ किना?
- ह्युमरस इन्टरलॉकिङ नेल छान्नु पर्दा के कारकहरूलाई माथी लिनु पर्दछ?
- ह्युमरस इन्टरलॉकिङ नेलहरूसँग सम्बन्धित केही सामान्य जटिलताहरू के हुन सक्छ?
- ह्युमरस इन्टरलॉकिङ नेलहरूबाट आउने कठिनाइहरूलाई कसरी प्रबंधन गर्न सकिन्छ?